Table of Contents
Introduction
In recent times, Brazil has faced a significant health challenge with the outbreak of the Oropouche virus. This virus, primarily transmitted through insect bites, has raised concerns due to its potential to spread from mother to fetus during pregnancy. Such vertical transmission can lead to severe outcomes, including stillbirths and congenital anomalies. Understanding the dynamics of this transmission is crucial for public health interventions and safeguarding maternal and fetal health.
Understanding the Oropouche Virus
The Oropouche virus (OROV) is an arbovirus belonging to the Bunyaviridae family. First identified in Trinidad and Tobago in 1955, it has since caused numerous outbreaks in South and Central America, particularly in Brazil. The virus is primarily transmitted to humans through the bite of infected biting midges, specifically Culicoides paraensis. Occasionally, mosquitoes like Culex quinquefasciatus have also been implicated in its transmission.
Symptoms and Clinical Manifestations
Oropouche virus fever typically presents with sudden onset of high fever, headache, muscle and joint pains, dizziness, photophobia, nausea, vomiting, and sometimes a rash. While most infections are self-limiting, resolving within a week, some cases can lead to neurological complications such as meningitis and encephalitis. Notably, recent observations have linked OROV infections during pregnancy to adverse fetal outcomes, including stillbirths and congenital anomalies.
Recent Outbreaks in Brazil
Since December 2023, Brazil has reported a surge in Oropouche fever cases, with over 9,852 infections documented. This outbreak has extended beyond the Amazon region, affecting urban areas and neighboring countries like Bolivia, Peru, Colombia, and Cuba. Alarmingly, this outbreak has recorded the first known fatalities attributed to OROV, highlighting its evolving pathogenicity.
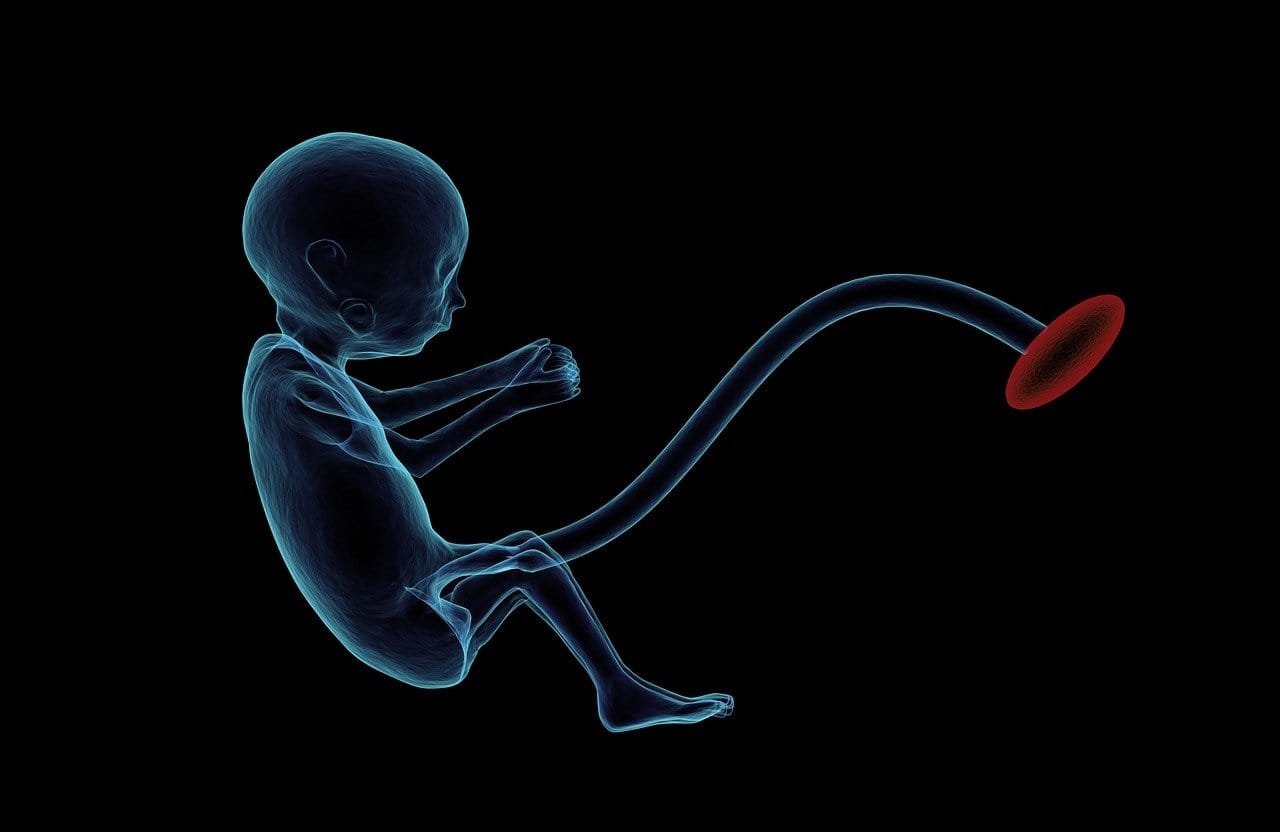
Vertical Transmission: From Mother to Fetus
Vertical transmission refers to the passage of a pathogen from a pregnant individual to their fetus during pregnancy or childbirth. In the context of OROV, recent studies have confirmed its ability to cross the placental barrier, leading to fetal infections. This mode of transmission has been associated with severe outcomes, including stillbirths and congenital anomalies such as microcephaly.
Case Studies Highlighting Vertical Transmission
In July 2024, Brazilian health authorities reported cases where pregnant women infected with OROV experienced adverse fetal outcomes. One notable case involved a 40-year-old woman who, at 30 weeks gestation, developed symptoms consistent with Oropouche fever. Subsequent investigations revealed the presence of OROV RNA in fetal tissues, confirming vertical transmission. These findings underscore the potential risks of OROV infections during pregnancy.
Mechanisms Facilitating Vertical Transmission
The exact mechanisms by which OROV crosses the placental barrier remain under investigation. However, it is hypothesized that the virus may infect placental cells, facilitating its entry into the fetal circulation. Factors such as the timing of infection during pregnancy and the maternal immune response may influence the likelihood and severity of vertical transmission.
Potential Risks to the Fetus
Fetal exposure to OROV can result in a range of adverse outcomes. These include intrauterine growth restriction, preterm birth, stillbirth, and congenital anomalies like microcephaly. The severity of these outcomes may depend on the gestational age at the time of maternal infection and the viral load transmitted to the fetus.
Diagnostic Approaches for OROV in Pregnant Women
Early diagnosis of OROV infection in pregnant women is crucial for managing potential risks to the fetus. Diagnostic methods include molecular techniques like reverse transcription-polymerase chain reaction (RT-PCR) to detect viral RNA, serological tests to identify specific antibodies, and ultrasound imaging to monitor fetal development and detect anomalies.
Treatment and Management Strategies
Currently, there is no specific antiviral treatment for Oropouche fever. Management focuses on symptomatic relief, including antipyretics for fever and analgesics for pain. In pregnant women, close monitoring of both maternal and fetal health is essential. In cases of confirmed vertical transmission, a multidisciplinary approach involving obstetricians, neonatologists, and infectious disease specialists is recommended to optimize outcomes.
Preventive Measures for Pregnant Women
Preventing OROV infection during pregnancy is paramount. Pregnant women are advised to avoid travel to areas with active outbreaks. If travel is unavoidable, protective measures include using insect repellents, wearing long-sleeved clothing, and staying in accommodations with proper screening or air conditioning to minimize exposure to biting midges and mosquitoes.
Public Health Implications
The potential for vertical transmission of OROV has significant public health implications. It necessitates heightened surveillance, especially among pregnant populations in endemic regions. Public health campaigns should focus on educating communities about transmission risks and preventive strategies. Additionally, healthcare systems must be equipped to manage and monitor affected pregnancies effectively.
Research and Future Directions
Ongoing research is essential to fully understand the mechanisms of OROV transmission and its impact on maternal and fetal health. Future studies should aim to develop specific antiviral therapies and explore vaccine development. Furthermore, investigating the ecological factors contributing to the spread of OROV can inform strategies to control its transmission.
Global Perspective on OROV Transmission
While OROV is primarily reported in South America, global travel and climate change may influence its distribution. International health organizations should collaborate to monitor and respond to potential outbreaks. Sharing data and resources can aid in developing comprehensive strategies to mitigate the impact of OROV on global health.
Conclusion
The recent Oropouche virus outbreak in Brazil has highlighted its potential to spread from mother to fetus, posing significant risks to both. This underscores the necessity for heightened surveillance, public education, and preventive measures, especially among pregnant women in affected regions. Healthcare providers should be vigilant in diagnosing and managing OROV infections during pregnancy to mitigate adverse outcomes. Ongoing research is essential to develop effective treatments and vaccines, aiming to curb the spread and impact of this emerging public health threat. Global collaboration and resource sharing are crucial to address the challenges posed by OROV and safeguard vulnerable populations.
FAQs
Q.1 What is the Oropouche virus?
A. The Oropouche virus (OROV) is an arbovirus primarily transmitted to humans through the bite of infected biting midges, particularly Culicoides paraensis. It belongs to the Bunyaviridae family and has been responsible for numerous outbreaks in South and Central America, especially in Brazil.
Q.2 How is the Oropouche virus transmitted?
A. OROV is mainly spread through the bites of infected biting midges. In some cases, mosquitoes like Culex quinquefasciatus have also been implicated in its transmission. Recent studies have shown that the virus can be transmitted from a pregnant mother to her fetus, a process known as vertical transmission.
Q.3 What are the symptoms of Oropouche fever?
A. Symptoms typically include sudden onset of high fever, headache, muscle and joint pains, dizziness, sensitivity to light (photophobia), nausea, vomiting, and sometimes a rash. While most infections resolve within a week, some cases can lead to neurological complications such as meningitis and encephalitis.
Q.4 What is vertical transmission, and why is it concerning with OROV?
A. Vertical transmission refers to the passage of a pathogen from a pregnant individual to their fetus during pregnancy or childbirth. In the context of OROV, this mode of transmission has been associated with severe outcomes, including stillbirths and congenital anomalies like microcephaly.
Q.5 How can pregnant women protect themselves from OROV?
A. Pregnant women are advised to avoid travel to areas with active OROV outbreaks. If travel is unavoidable, protective measures include using insect repellents, wearing long-sleeved clothing, and staying in accommodations with proper screening or air conditioning to minimize exposure to biting midges and mosquitoes.
Q.6 Is there a treatment or vaccine available for OROV?
A. Currently, there is no specific antiviral treatment or vaccine for Oropouche fever. Management focuses on symptomatic relief, including antipyretics for fever and analgesics for pain. Ongoing research is essential to develop effective treatments and vaccines to combat this emerging public health threat.
Q.7 How can OROV outbreaks be controlled?
A. Control measures focus on reducing the population of biting midges and mosquitoes through environmental management and insecticide use. Public health education campaigns are crucial to inform communities about preventive measures, such as eliminating standing water where these insects breed and using personal protective measures like insect repellents and bed nets.
Q.8 What should healthcare providers do when encountering a suspected OROV case?
A. Healthcare providers should consider OROV in patients presenting with symptoms consistent with the infection, especially if they have a history of travel to endemic areas. Laboratory testing can confirm the diagnosis. Providers should also report confirmed cases to public health authorities to aid in surveillance and control efforts.
Q.9 Can OROV be transmitted through blood transfusions?
A. While there is limited evidence on OROV transmission through blood transfusions, it is theoretically possible. Blood donation centers in endemic areas may implement screening measures to reduce this risk.
Q.10 What is the global impact of OROV?
A. Although OROV is primarily found in South and Central America, international travel can facilitate its spread to other regions. Global health organizations monitor OROV activity and provide guidance to prevent its spread and mitigate its impact on public health.